How to relieve persistent back pain?
With Emily Faragasso, Senior Physiotherapist
Have you ever experienced back pain? If so, you’re not alone. It is estimated that 84% of adults will experience at least one episode of back pain and that up to 23% of adults worldwide suffer from chronic low back pain. It is the leading cause of disability and the most common of non-infectious diseases.
Back pain can be classified by duration – acute (less than 6 weeks), subacute (6-12 weeks), and chronic (more than 12 weeks) – or by cause – mechanical (e.g. muscle strain), neuropathic (nerve-related), and non-mechanical/systemic (Infections, tumours, etc). There are many causes for back pain and symptoms are individual to each person. Additionally, clinicians cannot identify the specific cause for chronic low back pain in 90% of patients.
So, why does your low back hurt?
For a long time, pain was thought to be a sign of tissue damage. We now know, however, that pain is more of an alarm system. The human body has built in sensors that send signals to your spinal cord and brain when danger is sensed. The brain then decides whether you are actually in danger and, if it thinks you are, sends pain signals even if there is no actual damage. Sometimes this system can be hypersensitive, sending signals when there isn’t any harm, like when a smoke detector goes off when there’s a bit too much smoke from cooking but no fire.
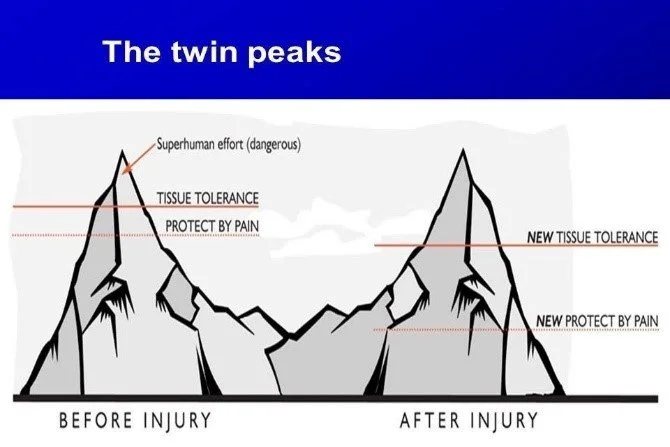
The Twin Peaks Model of pain shows how the alarm system can become more sensitized after an injury. Prior to an injury there is a smaller “buffer” between when your body experiences pain and when there is actual tissue damage. After an injury, however, not only does the tissue tolerance decrease, but the buffer zone becomes larger so that your body experiences pain with smaller movements. Understanding this change in sensitivity can help reassure that mild pain will not actually cause tissue damage and that learning how to gradually move through mild pain over time will dampen or desensitize the alarm system. This is particularly important with chronic pain, as we know that it’s incredibly important to continue to move to aid healing and recovery.
Why does pain persist?
Hypersensitivity of the nervous system, specifically the sympathetic nervous system (think fight or flight) can stay “switched on.” It is influenced and exacerbated by stress, emotional strain, poor sleep/fatigue, fear of movement, negative beliefs and negative reinforcement. Calming the nervous system, or activating the parasympathetic (rest and digest) system, is an important step in dialling down and desensitizing the pain response. Techniques include slow breathing or mindfulness, daily gentle movement, positive connection and laughter, and restorative sleep. Additionally, activity pacing, or moving/working around your pain threshold, is important in learning to move within your limits. That means moving within your tolerance and gradually increasing your activity level over time.
Why do I experience flare ups?
Healing isn’t linear or straightforward. Your body is re-learning how to move, the nervous system is still heightened and learning what is tolerable. Progress means shorter relapses, lower pain intensity, and increased activity tolerance. Though it’s easy to get frustrated by flare-ups or set-backs, try to maintain or return to a positive mindset, remembering that “pain is protection, not damage”. Resume calming strategies, gentle movement, and ensuring you get enough sleep, water, and nourishing food to help manage stressors.
What is the best treatment to help my recovery?
A recent systematic review on low back pain showed that exercise outperforms doing nothing, and that the specific type of exercise — whether Pilates, yoga, resistance training, aerobic work, or motor-control/stabilisation — didn’t change the outcome significantly. What does matter is consistent movement, progressive loading, and quality guidance.
This is exactly where we excel in supporting people with persistent back pain. Through clear education, close monitoring of symptoms, and thoughtful exercise progression, we help ensure you’re moving in ways that don’t amplify your pain. We guide you toward effective movement patterns and gradually build your exercise capacity so you can return to the activities you love with confidence.
Additionally, as discussed earlier, activity pacing, stress reduction, and learning to understand your pain. Know that your pain in real but start to identify what pain is tolerable and what pain is not. Seek treatment from your physiotherapist to learn how to move in ways that feel safe. The following are a few things you can do to heal.
· First line of treatment for non-specific back pain is to remain active
· Maintaining a healthy weight
· Avoiding activities that trigger symptoms
· Understand your pain is not always an indicator of tissue damage
Casiano V., et al. Back Pain. Stat Pearls. National Institute of Health. 11 Dec 2023 Back Pain - StatPearls - NCBI Bookshelf
Owen, P.,et al. Which specific modes of exercise training are most effective for treating low back pain? Network meta-analysis. Br J Sports Med. 2019 Oct 30; 54(21): 1279-1287.
Sullivan, M., & Vowles, K. (2017). The Twin Peaks Model of Chronic Pain: A Framework for Integrating Pain Management and Behaviour Change. Journal of Pain Research, 10, 2371–2380.